|
Only have a minute? Listen instead
Getting your Trinity Audio player ready...
|

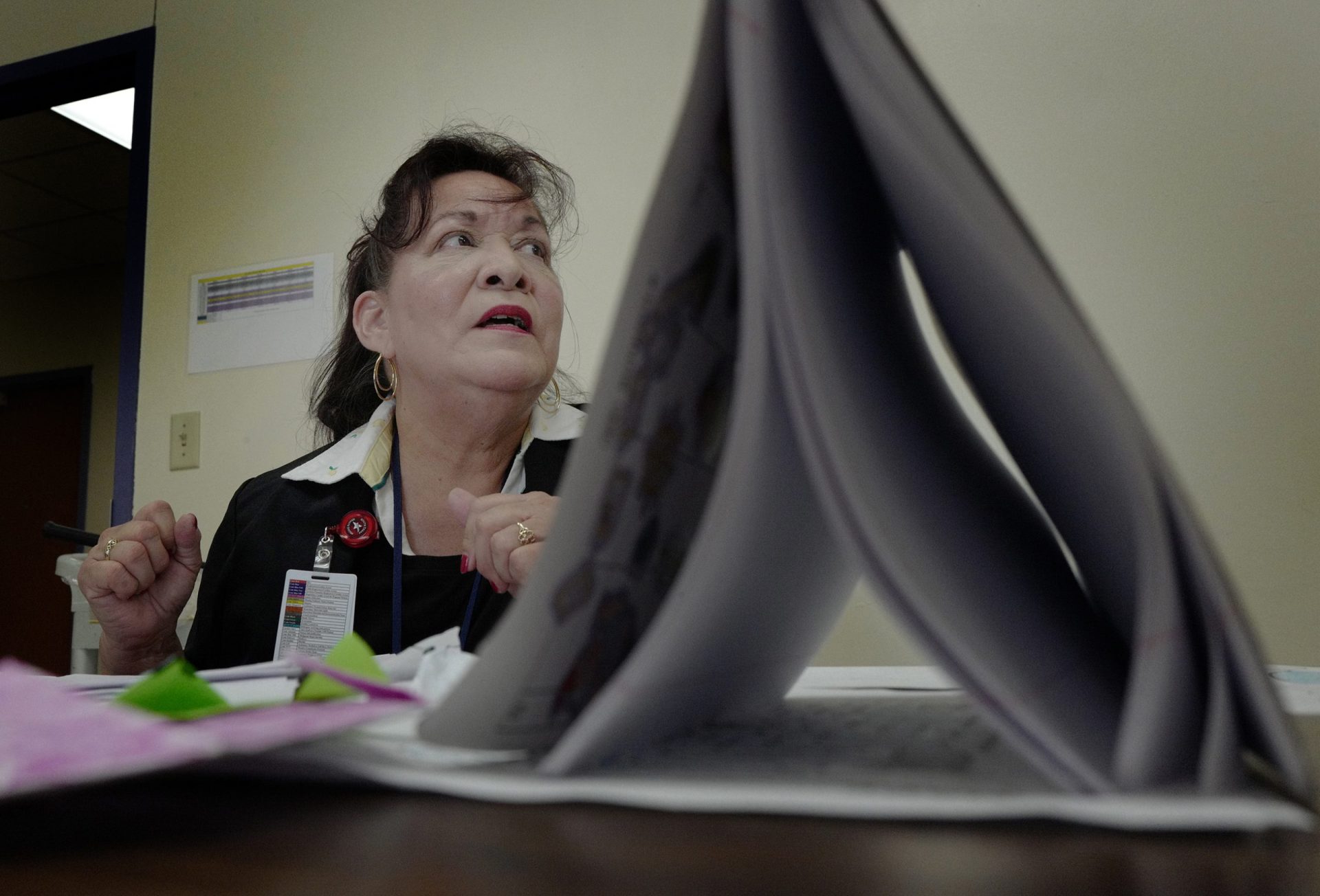
Rosalinda Jimenez was inspired to pursue a career that deals with mental health because of her father, who no one knew “was depressed until he mentioned it,” she said. Recollections of how her father, Isabel Jimenez, a World War II veteran, would “suffer in silence” and only spoke of his experience late in his life helped her realize the toll that war took on his mental health, and that there are many like him who still struggle.
“I didn’t want anybody else to worry, I didn’t want anybody else to suffer,” she recalled him saying when asked why he hadn’t told anyone about the trauma, which can be common for combat war veterans who have difficulty sharing their experiences.
It wasn’t until toward the end of his life that her father — a World War II veteran and a Navy Purple Heart recipient — began to open up about his time in war and the struggles that continued after returning.
Now years later, Jimenez — herself a ground radio operator for the U.S. Air Force for two years — is equipped not just in expertise but in her own military experience to help as a therapist at South Texas Health System Behavioral.

In fact, to say she is inspired to help other veterans who struggle with mental health issues such as posttraumatic stress disorder, or PTSD, would be quite the understatement.
According to the U.S. Department of Veteran Affairs, mental health conditions like PTSD are slightly more common in veterans than civilians with about 7 of 100 veterans, or 7%, who struggle with PTSD. The VA also reported that veterans made up 18% of suicides in the U.S. in 2014.
The VA has further identified that PTSD can be three times more likely among those who are deployed, and factors include combat situations but also ranges from military occupation or specialty to the politics around a war, as well as where the war is fought and the enemy that’s faced.
Citing a “large study of veterans across the country,” the VA reported that 15 out of 100 veterans of Operations Iraqi Freedom and Enduring Freedom reported suffering from PTSD in the past year, or 15%. That number rises to 29% for veterans who experienced it at some point in their life.
Their data shows a decline in veterans of previous wars reporting PTSD, with 14% and 21% of Persian Gulf War veterans reporting it in the past year and at some point in their life, respectively; 5% and 10% of Vietnam veterans; and 2% and 3% of WWII and Korean War veterans.
“There’s a lot of hurt out there you know, and they just need somebody to reach out to and know that somebody is there to listen to them — veteran or not,” Jimenez said in a June 9 interview to shed more light on mental health matters, and in observance of June being PTSD Awareness Month in the U.S.
She explained that it is common especially in combat veterans to avoid talking about mental health issues, as many even avoid saying the word depression.
“That happens, they just don’t want to say the word,” Jimenez said, adding that she believes it is due to a sense of pride.
Some choose not to reach out for help because they are taught that they have to remain strong and therefore believe they should endure their mental health on their own.
However, Jimenez wants to remind those who served that it’s OK to ask for help.
“There is nothing wrong with saying, ‘Yeah, maybe I do need some help,’ and that’s why we are there for them.” she said.
HOW TO GET HELP
Jimenez said STHS Behavioral is implementing the Veterans Comprehensive Prevention, Access to Care, and Treatment Act — or the COMPACT Act of 2020 — which will provide veterans in a suicidal crisis with free emergency care.
Those who qualify for this free care do not have to be enrolled in the VA to receive it; however, they must have been honorably discharged and must have served for at least 24 months.
Through the act, STHS Behavioral will provide each veteran with 30 days of inpatient care where they will help “stabilize them.” The health system will then refer them to outpatient care for 90 days.
Along with patient care at STHS, Jimenez explained that other resources are also available through the VA, where researchers are improving treatment for depression “by probing the biological roots of the condition” and “exploring the benefits and risks of a wide variety of existing and potential new treatments,” according to the VA’s Office of Research & Development.
Veterans can also chat online with trained counselors at www.VeteransCrisisLine.net.
Services are available for transitioning service members, for veterans looking for support, women veterans, LGBTQ+ veterans, for family members or friends, for older veterans and healthcare providers as well as college faculty members.
A toll-free, confidential crisis line staffed by mental health professionals has also been set up for veterans and can be reached by calling (800) 273-8255, or (800) 273-(TALK). There is also a text line open at #838255.
Not only does the VA help veterans but their families by providing information on how they can help their loved ones. Resources for those families are also available at the VA.








